Study area, design and population
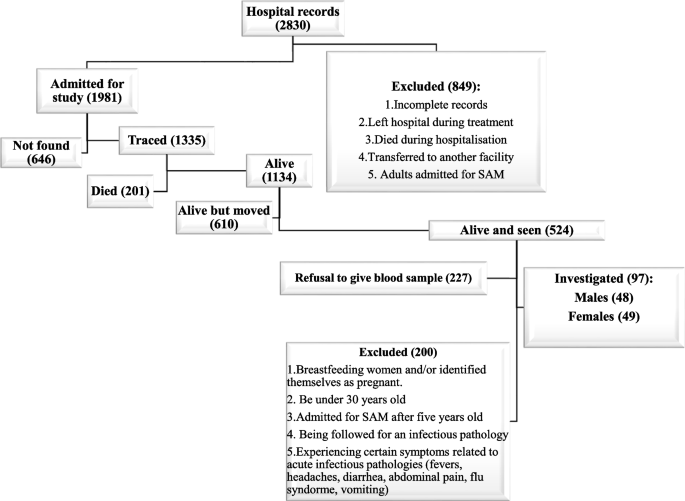
This was a follow-up observational study comparing adults with a history of hospitalization for SAM with community-dwelling control adults. Adults who were treated for SAM during childhood at Lwiro Pediatric Hospital (LPH) between 1988 and 2007, and still living in Miti-Murhesa and Katana Health Zone (HZ) in 2018, were assessed (38, 39). A total of 1981 children were treated for SAM at LPH during the above period (39). The nutritional status of study participants at the time of hospital admission (37, 39, 40) was reassessed with the Emergency Nutrition Assessment (ENA) for the SMART program (October 2007 version) based on the WHO child growth standards (4). Based on these standards, 1664 children were classified as having suffered from SAM (39). The others were excluded from further analyses. All children hospitalized for SAM were treated according to the guidelines used at the time (37). For the initial follow-up group, 524 participants from the initial cohort still residing in the two ZS were examined (38). To assess the long-term consequences of SAM on growth and health, these survivors (exposed to SAM) were compared to 407 unexposed control adults, randomly selected from the same community (38, 39).
The inclusion criteria for individuals exposed to SAM for this study were as follows: being at least 30 years old, having suffered from SAM before the age of 5 years, and voluntarily agreeing to participate in the study.
To be included, unexposed controls must have the following characteristics: no hospital history of SAM, be of the same sex as matched participants, live in the same community, and be less than 24 months older or younger than exposed participants. Unexposed individuals were randomly selected by spinning a bottle at the exposed participant’s home and going door to door, starting at the closest house the bottle was pointing toward (38, 39).
Based on these criteria, 97 adults with previous SAM were included and formed the exposed group, and matched with 97 unexposed control adults among the potential participants (524 exposed and 407 unexposed) (Fig. 1).
The exclusion criteria for the study were: breastfeeding women and those identifying as pregnant (more than 3 months of amenorrhea or with visible pregnancy), and being followed for an infectious pathology or presenting certain symptoms linked to pathologies acute infectious diseases (fevers, headaches, diarrhea). , abdominal pain, flu syndrome, vomiting) during the previous two weeks.
Variables
Dependent variables
Our primary outcomes of interest were hematological disorders, including anemia, leukopenia, leukocytosis, thrombocytopenia as well as increased platelet counts in adulthood, assessed by standard laboratory measures (count of blood cells and erythrocyte parameters). We evaluated the associations between exposure to SAM during childhood and red blood cell levels (red blood cells (RBC), hemoglobin (Hb) as well as erythrocyte constants: mean corpuscular volume (MCV), mean concentration of corpuscular hemoglobin (MCHC) and mean corpuscular hemoglobin content (MCH), white blood cells (white blood cells (WBC) and leukocyte count (neutrophils, lymphocytes and eosinophils)) and platelets.
Anemia was defined as Hb < 13.0 g/dL in men and < 12.0 g/dL in women; leukopenia like WBC <3 500 WBC/μL, tandis que la leucocytose a été définie comme WBC >11,000 WBC/μL. Thrombocytosis was defined as a platelet count < 150 000/μL, alors qu'une augmentation du nombre de plaquettes a été définie comme > 450,000/μL.
BMI (body mass index) was calculated as weight/height2 (in kg/m2) and classified into four categories: <18.5 = underweight, 18.5 to 24.9 = normal, 25 to 29.9 = overweight and ≥ 30.0 = obesity.
Independent variables
For hematological disorders and their various biological markers, the main exposure was a history of SAM in childhood. Lifestyle (food consumption) was added to the modeling as a potential confounding factor.
Food consumption frequency was assessed using a dietary diversity score (DDS) designed by the World Food Program (WFP) (29, 41, 42). This score measures household dietary diversity, weighted by frequency of consumption. The head of household (often the mother) is asked how many days in the last seven days the household consumed one of the following 10 food groups (cereals, tubers, legumes, vegetables, fruits, meat/fish, milk/ dairy products, sugar). , oil/fat, condiments). Then, the frequency of consumption of each food group was multiplied by its nutritional value, to obtain a score per food group. Finally, the scores for each food group were added together to obtain an overall score.
Based on this overall score, a subject was considered to have an inadequate, borderline or satisfactory diet if the score was between 0 and 28; 28.5-42 and >42, respectively (29, 42).
Data gathering
Data collection lasted approximately four months (August-November 2020) and was carried out in two stages by trained community health workers (CHWs). It was led by district authorities, head nurses and community relays. The CHWs involved in data collection were the same people who participated in the identification of subjects during the reconstitution of the exposure cohort (39).
The first step was a home visit. During these visits, CHWs gave participants a questionnaire translated into Kiswahili and took their anthropometric measurements. Participants were given an appointment at the nearest hospital for the second stage of data collection, within 48 hours. This second step consisted of having a venous blood test carried out by qualified local nurses.
Unlike nurses and lab workers who did not know whether a participant was exposed or not, CHWs knew this information. However, to avoid subjectivity and bias in the results, the context of demographic data collection was presented as part of a routine exercise rather than a comparison between exposed and unexposed.
The questionnaire included variables relating to participant identity, anthropometric parameters and food consumption.
The anthropometric parameters considered were weight and standing height. Anthropometric measurements were performed in accordance with WHO guidelines (4) and were quality checked by having two team members independently measure anthropometric parameters. The coded figure was the average of these two measurements. If there was a difference of more than 300 g for weight and/or 0.5 cm for standing height, a third measurement was taken and the average of the two closest measurements was used.
Finally, 4 ml of blood were obtained from an antecubital venipuncture after 12 hours of fasting for the determination of the complete blood count after counting on an automatic machine using standard enzymatic calorimetric methods (CYAN smart CY009, Brussels, Belgium) in the laboratory. of the Provincial General Assembly of Bukavu. referral hospital (tertiary level hospital).
statistical analyzes
We used Stata version 13.1 software for statistical analyses. Categorical variables are summarized by frequency and proportion. Continuous variables are presented as mean and standard deviation (SD), as they all had a symmetric distribution.
Pearson’s chi2 or Fisher’s exact test (if the conditions of application of Chi2 were not satisfied) were used to compare categorical variables and Student’s t test to compare means between groups.
Linear and logistic regression models were used for continuous variables (WBC, neutrophils, lymphocytes, red blood cells, platelets, Hb and hematocrit (Hct), MCV, MCHC and MCHC) and categorical variables (anemia, thrombocytopenia, leukopenia, increased platelets and leukocytosis). respectively. Baseline models included only the primary exposure: SAM, thus providing a raw mean difference between exposed and unexposed for quantitative variables, and crude odds ratios (OR) for categorical variables. Mean differences and ORs are presented with 95% confidence intervals (95% CI).
To assess the potential confounding effect of adult dietary habits on the hematological profile, we added the food consumption score to the adjusted model. To be included in the models, food consumption was dichotomized. We considered that people with a satisfactory level of dietary diversity were those with a reasonable food consumption score. The other categories were considered to have a “low” level.
It should be noted that the conditions for applying linear regression (normality, homoscedasticity and linearity) were verified by residual analysis and that the quality of fit of the logistic model was verified by the Hosmer-Lemehow test.