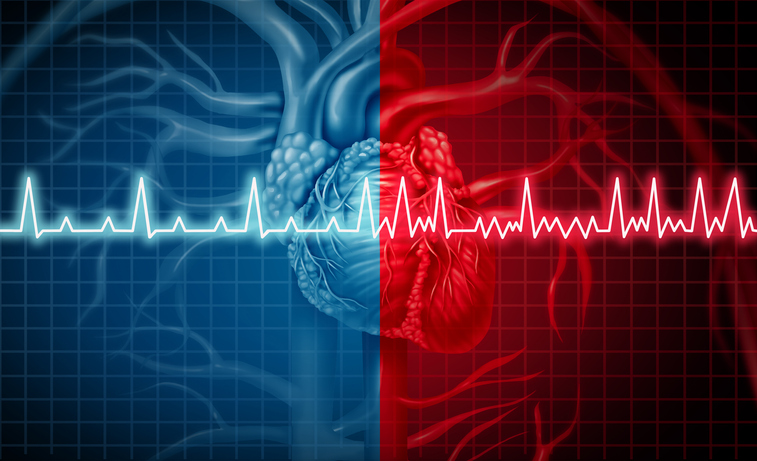
The American College of Cardiology (ACC) and the American Heart Association (AHA), in collaboration with other medical associations, have released new comprehensive guidelines for the prevention and management of atrial fibrillation (Atrial fibrillation). Published simultaneously in the Journal of the American College of Cardiology And TrafficThe guideline addresses how doctors should treat patients with atrial fibrillation, an increasingly common condition that already affects more than six million people in the United States.
The updated recommendations emphasize a multifaceted approach, incorporating lifestyle modifications, early rhythm control strategies, and advances in therapeutic interventions. If left untreated, atrial fibrillation can lead to exacerbated heart failure and also significantly increase the risk of stroke.
A notable change in the new guidelines is a new stage-based classification system for atrial fibrillation, which no longer relies solely on the duration of the arrhythmia. This change emphasizes the disease continuum and promotes a holistic, multidisciplinary management approach. The guideline recognizes atrial fibrillation as a complex cardiovascular disease requiring various strategies at different stages, including prevention, lifestyle modification, screening and therapy. It also provides advice on medications that regulate patients’ rhythm and frequency, the use of blood thinners, and when to suspend or discontinue use of these medications.
“It’s a complex disease. This is not just an isolated heart rhythm disorder, and we now know that the longer a person is in atrial fibrillation, the more difficult it is to return them to normal sinus rhythm,” said Jose Joglar, MD. , professor of cardiac electrophysiology at UT Southwestern. Medical Center of Dallas and Chairman of the Editorial Board. “The new guideline reinforces the urgent need to address atrial fibrillation as a complex cardiovascular disease that requires disease prevention, risk factor modification, as well as optimization of therapies and patient access to long-term care and management.”
The new guidelines detail some specific approaches to managing and treating atrial fibrillation, including:
Lifestyle modifications and prevention-The guideline emphasizes healthy lifestyle habits to prevent or alleviate the burden of atrial fibrillation. Jose Joglar, MD, chair of the editorial board, emphasizes the need for prescriptive recommendations, saying, “Many patients don’t know where to start when given advice about changing their lifestyle, so we are very precise in our recommendations. » This includes targeted advice on weight loss, obesity prevention, physical activity, smoking cessation, limiting alcohol consumption and controlling blood pressure and other comorbidities . The goal is to empower clinicians to provide patients with clear, achievable goals for healthier living.
Catheter ablation as first-line therapyBased on recent data supporting its effectiveness over medications in preventing disease progression, the guideline elevated catheter ablation to a Class 1 treatment recommendation for properly selected patients. This is a change from the traditional approach of considering it as a second-line option after drug treatment. Catheter ablation, a minimally invasive procedure that deactivates irregular heart tissue, is now advised as a first option in some patients with atrial fibrillation, particularly those with heart failure with reduced ejection fraction.
Stroke prevention and risk stratification –While endorsing the continued use of the CHA2DS2-VASc score to assess stroke risk, the guideline allows flexibility in incorporating other risk calculators where uncertainty exists or risk factors Additional information must be taken into account. Kidney diseases, for example, not included in CHA2DS2-VASc, can be assessed using alternative tools. The guideline encourages clinicians to evaluate patients at intermediate risk using multiple risk calculators to make informed decisions regarding anticoagulant prescriptions.
Left atrial appendage closure devices-The guidelines also recommend greater use of left atrial appendage closure devices for stroke prevention. These devices, placed in the left atrial appendage of the heart, prevent blood clots from entering the bloodstream. This recommendation reflects technological advances and the potential benefits of these devices in certain patient populations.
The new ACC/AHA guideline on atrial fibrillation aims to provide guidance to physicians on new treatment modalities without being rigid, Joglar noted. “The new guidelines give clinicians the opportunity to use other predictive tools, and we hope this will also improve communication and shared decision-making with patients,” he said.
Similar to other chronic diseases, such as high blood pressure or type 2 diabetes, Joglar added that we “now have better understanding and more tools to prevent, treat and also mitigate the risk of atrial fibrillation so we can improve patient outcomes.”