The COVID-19 pandemic has posed significant challenges to health systems and access to care in the United States, including for people living with HIV and the systems that serve them. To better understand the impact of the pandemic on HIV, we surveyed Ryan White providers funded directly by the country. Ryan White, the federal HIV protection program, serves more than half of those diagnosed with the disease nationwide, providing outpatient care and HIV-related support services. Our main conclusions are as follows:
- Respondents described an immediate shift toward new ways of providing HIV care and prevention during the early months of the pandemic.
- Nearly all now offer telehealth services (99%), compared to 22% in the past, and on average conduct about half of patient visits virtually. However, the “digital divide” means that telehealth services are not an option for all patients.
- Most (89%) offer multi-month antiretroviral (ARV) prescriptions, and half said this practice has increased due to COVID-19.
- Seven in ten (70%) conduct on-site COVID-19 testing.
- Nearly a third (30%) reported an increase in new customers and almost 40% of respondents saw a change in payer mix, primarily an increase in uninsured customers, followed by losses private coverage, followed by an increase in the number of clients receiving Medicaid.
- Respondents report that clients are facing significant stress and uncertainty amid the pandemic, noting, among other challenges, worsening mental health, job losses, and reduced access to support services.
- Respondents also faced significant challenges related to staffing. More than a quarter (27%) reported staff layoffs or furloughs and the same proportion reduced staff hours. Additionally, staff morale was a challenge reported by three-quarters (74%) of respondents.
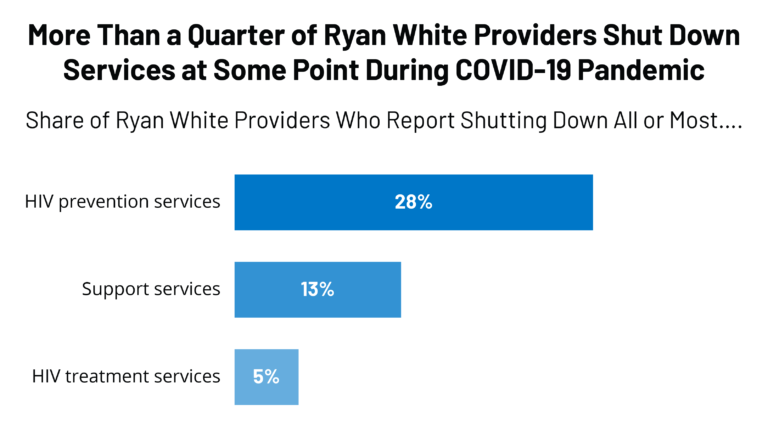
- Operational difficulties were common, including for the 28% who closed all or most of their HIV prevention services in response to the pandemic. Other challenges included difficulty connecting with service partners and increased costs.
- Following COVID-era public health guidelines remains a challenge for some who suffer from inadequate clinical space for social distancing (32%), insufficient access to COVID-19 testing (22%), and insufficient PPE (10%).
- However, despite these historical challenges, most respondents report having adapted to a “new normal” and showing great resilience in adapting to new ways of providing care.