
Chronic pain affects nearly a third of the U.S. population, according to a 2011 study. report by the Institute of Medicine to advance pain research, care and education. In recent years, the use of prescription medications to manage pain has increased exponentially. These drugs have not only proven to be largely ineffective, but they also expose millions of people to highly addictive medications that often lead to substance use disorders and even death.
Increasingly, non-pharmaceutical approaches, including physiotherapy, are recommended as “first-line treatment” for pain management.
The Centers for Disease Control and Prevention (CDC) published a set of guidelines in March 2016 with the goal of limiting opioid prescriptions to cancer treatments, palliative care, end-of-life care and certain emergency situations. For other pain management, the CDC recommends “non-opioid approaches,” such as physical therapy.
Even when opioids are prescribed, the CDC recommends that patients receive the lowest effective dose and that it be combined with physical therapy or other “non-opioid” treatment.
“Physical and occupational therapists can play an important role in pain management,” says Gina Ruppert, PT, CLT, a physical therapist at Chester County Hospital. “We have many tools in our arsenal that don’t involve medications. And although physical therapy is often thought of as exercise or massage, it is more accurate to think of it as a progressive and holistic approach.
Incorporating alternative approaches to address prescription drug overuse is not new to the healthcare system. Experts in specialties such as emergency medicine, behavioral economics, orthopedics, plastic surgery, obstetrics and gynecology, and psychiatry have been working for years to reduce the number and doses of drug prescriptions. opioids administered to patients through the development of new procedures and protocols. And two years ago, Penn Medicine created Health System-wide opioid task forceestablishing itself as a leader in the fight against opioid addiction.
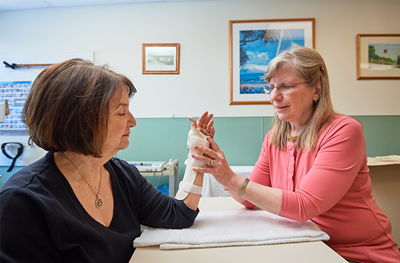
Jill Townsend, physiotherapist, CHT, senior hand therapist at Chester County Hospital, says the treatment provided by physical therapists is a collaborative effort with their patients and health care providers.
“We first identify the cause of their pain, then we work to help them understand their diagnosis and develop tools to help them manage their pain,” she says. “In the vast majority of cases, we manage to resolve the problem. In chronic cases, patients have the tools to manage and control their discomfort.
This work is not entirely physical. Part of the effort involves helping patients identify potential emotional or environmental triggers for their pain. Stress, for example, can increase physical discomfort, so Townsend and Ruppert help patients practice stress management principles through breathing, visualization and relaxation techniques.
The physical aspect of pain can also be addressed through a variety of approaches that can improve circulation, decrease swelling, reduce muscle spasms, and treat pain. These include heat, cold, ultrasound and electrical stimulation. Manual therapy (massage, mobilization, and manipulation of joints and soft tissues) has also been shown to be effective in utilizing the body’s ability to control pain.
Patients receive an individualized exercise program that helps address their specific strength and flexibility deficits. Aerobic exercise, in particular, is another way to use the body’s defenses against symptoms. Therapists also provide ergonomic training, sleep education and movement analysis, where the patient learns to move, sit and stand more effectively.
“While we have general guidelines and indications, it’s all based on clinical reasoning, which is understanding the science of the patient’s pathology and implementing an individualized plan,” says Townsend. In other words, each patient’s treatment is tailored to their particular needs and abilities. A constant and open dialogue between therapist and patient is an integral part of this process.
“Often, during treatment, their pain evolves. It could even happen daily,” says Ruppert.
The challenge, Townsend says, is getting patients to respect their pain without overanalyzing it. “Focusing too much on pain can increase pain. »
As the role of the physical therapist continues to evolve and complement current care protocols, it will allow patients to benefit from more holistic and comprehensive therapies for a variety of conditions.
