Each week, we identify a top search term, speculate on the causes of its popularity, and provide an infographic on a related condition. If you have any thoughts on what’s trending and why, share them with us on Twitter Or Facebook.
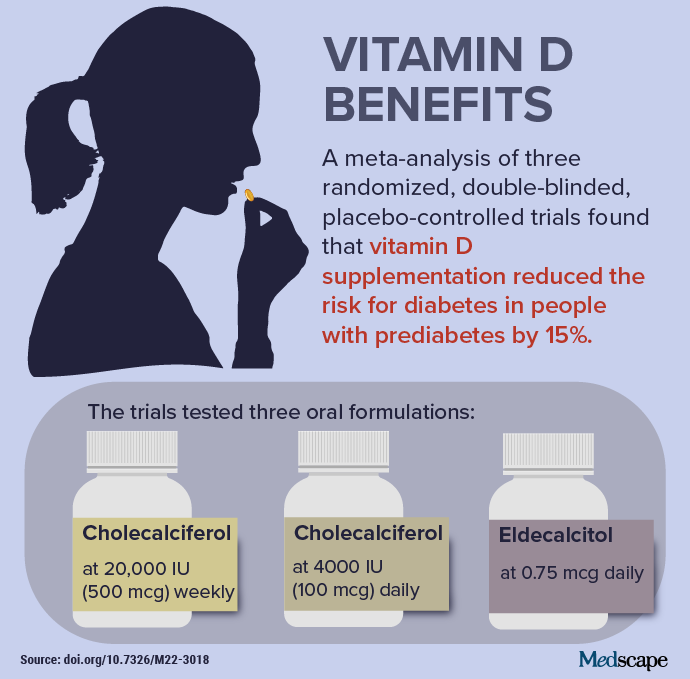
The potential benefits of vitamin D are the subject of frequent research. New studies have investigated whether supplementation can prevent diabetes, reduce suicide attempts, and lower the risk of melanoma. Promising results helped spark interest in this week’s top trending clinical topic. In results published in early February, researchers detailed the impact of vitamin D. in prediabetic patients (see Infographic).
Researchers found no difference in adverse event rate ratios (kidney stones, 1.17 (95% CI, 0.69-1.99); hypercalcemia, 2.34 (95% CI, 0.83-6.66) hypercalciuria, 1.65 (95% CI, 0.83-3.28); death, 0.85 (95% CI, 0.31-2.36) among participants who received vitamin D and those who received a placebo. The authors acknowledged that the absolute risk reduction figure is small (3.3%) and confirmed that intensive lifestyle changes and metformin remain more effective interventions. However, they noted that “extrapolation to the more than 374 million adults with prediabetes worldwide suggests that inexpensive vitamin D supplementation could delay the development of diabetes in more than 10 million people.”
The authors also suggest that the optimal level of vitamin D in the blood needed to reduce the risk of diabetes may be higher than previously thought. “(T)he blood level of 25-hydroxyvitamin D needed to optimally reduce the risk of diabetes may be close to or even higher than the range of 125 to 150 nmol/L (50 to 60 ng/mL) that the Committee The Institute of Medicine’s Diet Review Guide published in 2011. Reference intakes for calcium and vitamin D correspond to the Tolerable Upper Intake (UL) range of 4,000 IU/day for the vitamin D,” the authors said.
A accompanying editorial calls for caution regarding dosage. These authors note that “vitamin D supplementation of 10 to 20 mcg (400 to 800 IU) per day can be safely applied at the population level to prevent skeletal, and possibly non-skeletal, diseases.” Treatment with very high doses of vitamin D could prevent type 2 diabetes in some patients, but can also cause harm.
Other encouraging news, supplementation almost half the suicide rate and intentional self-harm among US veterans with vitamin D deficiency. The effects were even stronger among black veterans. A retrospective cohort study reviewed the records of 1.3 million veterans and found 490,885 veterans who received vitamin D3 (cholecalciferol) and 169,241 who received vitamin D2 (ergocalciferol). These patients were compared individually to veterans of similar demographics and medical history who did not receive supplementation.
Unadjusted rates of suicide attempts and intentional self-harm were 0.27% for those who took vitamin D2 compared to 0.52% for those who did not take the supplement. For vitamin D3, the levels were 0.20% versus 0.36%, respectively. Vitamin D2 supplementation was associated with a 48.8% reduction in suicide/self-harm risks. Vitamin D3 was associated with a 44.8% reduction. Risk reductions were similar between men and women; however, supplementation had a greater effect among black veterans (57.9% reduction for vitamin D2, 63.8% for vitamin D3) compared to white veterans (46.3% for vitamin D2, 38.7% for vitamin D3). These results only applied to those with insufficient vitamin D levels. Among those with levels ≥40 ng/mL, no significant overall or dose-response association with risk of suicide attempt/self-harm was observed.
Vitamin D may also help reduce the risk of melanoma. A Finnish study found that people who regularly take supplements are much less likely have malignant melanoma or skin cancer of any type. The study involved nearly 500 people. Regular vitamin D users saw a significant 55% reduction in melanoma diagnosis. Occasional drinking was associated with a non-significant reduction of 46%. The reduction was similar for all types of skin cancer. However, lead author Ilkka T. Harvima, MD, PhD, cautioned that the study had limitations. Despite controlling for several possible confounding factors, “it is still possible that other factors, as yet unidentified or untested, could still confound the current result,” he said.
An important caution from a separate study: response to vitamin D supplementation can be blunted in overweight or obese patients. A new post hoc analysis reviewed the Vitamin D and Omega-3 Large-Scale Trial (VITAL). VITAL found no overall benefit associated with vitamin D supplementation (2,000 IU/d) for 5 years in terms of cancer or major cardiovascular diseases. However, secondary analyzes prespecified by body weight showed that patients with a healthy weight (BMI < 25) had significant benefits compared to placebo in terms of cancer incidence (24% lower), mortality from cancer (42% less) and autoimmune diseases. (22% less). Among the main theories as to why a higher BMI would be linked to reduced benefits of vitamin D supplementation, since vitamin D is a fat-soluble vitamin, increased adiposity and fat storage capacity associated with higher BMI results in more great elimination of the vitamin from the circulation.
From diabetes to suicide and skin cancer, the potential for interventions involving vitamin D supplementation remains promising. Even with caveats and concerns, such as possible reduced effectiveness in people with higher body weights, the promise of these recent findings has resulted in this week’s top trending clinical topic.
Take a quiz about vitamin D.