Each week, we identify a top search term, speculate on the causes of its popularity, and provide an infographic on a related condition. If you have any thoughts on what’s trending and why, share them with us on Twitter Or Facebook.
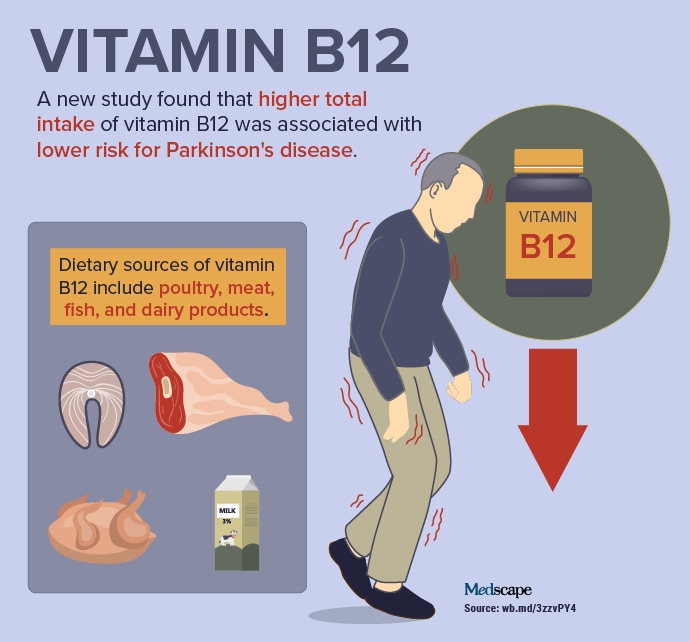
The potential benefits of vitamins are still a hot topic. New findings suggesting that vitamin B12 is associated with possible protection against Parkinson’s disease, ALS progression, and the severity of fatty liver disease have recently attracted increased interest. At International Congress on Parkinson’s Disease and Movement Disorders (MDS) 2022the researchers presented their results of a study this included more than 80,000 women and almost 50,000 men. The analysis included information on dietary, supplemental and total intake of folate, vitamin B6 and vitamin B12 over a period of approximately 30 years, through 2012 (see infographic).
During follow-up, 495 women and 621 men were diagnosed with Parkinson’s disease. Investigators adjusted for potential confounders including age, year, smoking, physical activity, alcohol or caffeine use, hormone use (in women), drug use dairy products and flavonoids and the Mediterranean diet score. Participants with higher total vitamin B12 intake had a lower risk of Parkinson’s disease (pooled hazard ratio for the highest versus the lowest quintile, 0.74; 95% CI, 0.60-0. 89; P. for trend, .001). Intake from both diet and supplements contributed to this inverse association. To try to overcome the risk of reverse causality, the researchers examined vitamin B12 intake during four staggered exposure periods: 8, 12, 16 and 20 years. They found a significant relationship between drinking over a 20-year period and the development of Parkinson’s disease. Overall, the results support a possible protective effect of early vitamin B12 intake on the development of PD.
In a separate study earlier in 2022, an ultra-high dose of methylcobalamin, an active form of vitamin B12 analogue, was found to slow functional decline by 43% in patients with early-stage amyotrophic lateral sclerosis (ALS) . The 50 mg dose was administered twice a week by intramuscular injection. In the phase 3 study, effectiveness was higher in participants who also took riluzole, a drug approved by the U.S. Food and Drug Administration to treat ALS. The study included outpatients from 25 neurology centers in Japan who were diagnosed with definite or probable ALS and whose symptoms began within the previous year. After 12 weeks of observation, the 130 participants who remained ambulatory and showed a decrease of only 1 or 2 points in the total score of the amyotrophic lateral sclerosis functional rating scale-revised (ALSFRS-R) were enrolled in a period treatment period of 16 weeks.
These patients (mean age: 61 years; 56.9% male) were randomly assigned to receive 50 mg of methylcobalamin or placebo. The primary endpoint was change in ALSFRS-R total score. At 16 weeks, this total score was -2.66 in the methylcobalamin group and -4.63 in the placebo group (95% CI, 0.44-3.50; P. = 0.01). In the 90% of patients also taking riluzole, the difference in favor of methylcobalamin was even greater (-2.11; 95% CI, 0.46-3.76; P. = 0.01). The difference in ALSFRS-R total score between active drug and placebo was 43% in all patients and 45% in those using riluzole. Adverse events (AEs) were experienced by 62% of patients receiving the drug and 66% of patients receiving the placebo. AEs reported by at least 5% of patients in both groups included constipation, nasopharyngitis, bruising, falls, back pain, and insomnia. No AEs led to treatment discontinuation.
Another study found that vitamin B12 and folic acid may also play a role in preventing or delaying the progression of nonalcoholic steatohepatitis (NASH). The researchers found that high blood levels of homocysteine are strongly correlated with disease severity. However, the precise relationship between hyperhomocysteinemia and NASH is poorly understood. In their new study, Singh and colleagues determined that as hepatic homocysteine levels increase, amino acids attach to various liver proteins, changing their structure and hindering their function. In particular, when homocysteine attaches to the protein syntaxin 17, it prevents the protein from transporting and digesting fats (a process known as autophagy). This, in turn, induces the development and progression of hepatic steatosis to NASH. In preclinical models, researchers have found that vitamin B12 and folic acid supplementation increases hepatic syntaxin 17 levels, restores its role in autophagy, slows the progression of NASH, and reverses inflammation and fibrosis. liver.
From Parkinson’s disease to ALS and NASH, recent studies suggesting the importance of vitamin B12 have recently gained attention, leading to this week’s top trending clinical topic.
Take a quiz on the use of vitamin B12.